They are diagnoses that no one wants to hear: heart failure, stroke, heart attack.
Heart-wrenching words – in more ways than one – that make up what we call cardiovascular disease, or CVD.
Most of us have a personal connection with CVD – a friend whose life was cut too short, or a family member who was able to identify risk factors early on and make lifestyle changes.
While the field of cardiology continues to grow, there’s still a lot to learn about the leading cause of death among men and women worldwide.
That’s where UNC Greensboro comes in. It’s the kind of research that falls right in our sweet spot – real-world, high-impact, with scientists working across disciplines and with community partners to improve health and wellness in our state and beyond.
UNCG researchers are coming at this problem from a variety of angles. One group is working on a device to monitor CVD risk and identify a heart attack when it’s happening. Another team is investigating how self-regulatory behaviors in early childhood affect cardiometabolic risk later in life. Other researchers are targeting interventions for specific populations, such as women and individuals with type 1 diabetes.
Call it a campus-wide assault on CVD – one that’s poised to make an impact.
Tick-Tock
During a heart attack, the phrase “every minute matters” is not a cliché. It’s a harsh reality with what can be deadly consequences.
Cardiologists will tell you that “time is muscle.” The longer you wait before getting treatment for a heart attack, the more heart tissue dies.
Typically, when emergency personnel arrive at the scene of someone experiencing heart attack symptoms, they use an electrocardiogram, or EKG, to measure the heart’s electric activity and determine if a heart attack is taking place. But here’s the catch: For about half of individuals experiencing a heart attack, an EKG won’t detect abnormalities.
If the EKG confirms a heart attack, emergency personnel can activate a system in which the hospital swiftly prepares for the incoming patient. If not, the patient has to go through the emergency department and do additional testing to confirm the heart attack.
Meanwhile, tick-tock goes the clock. And more heart muscle dies.
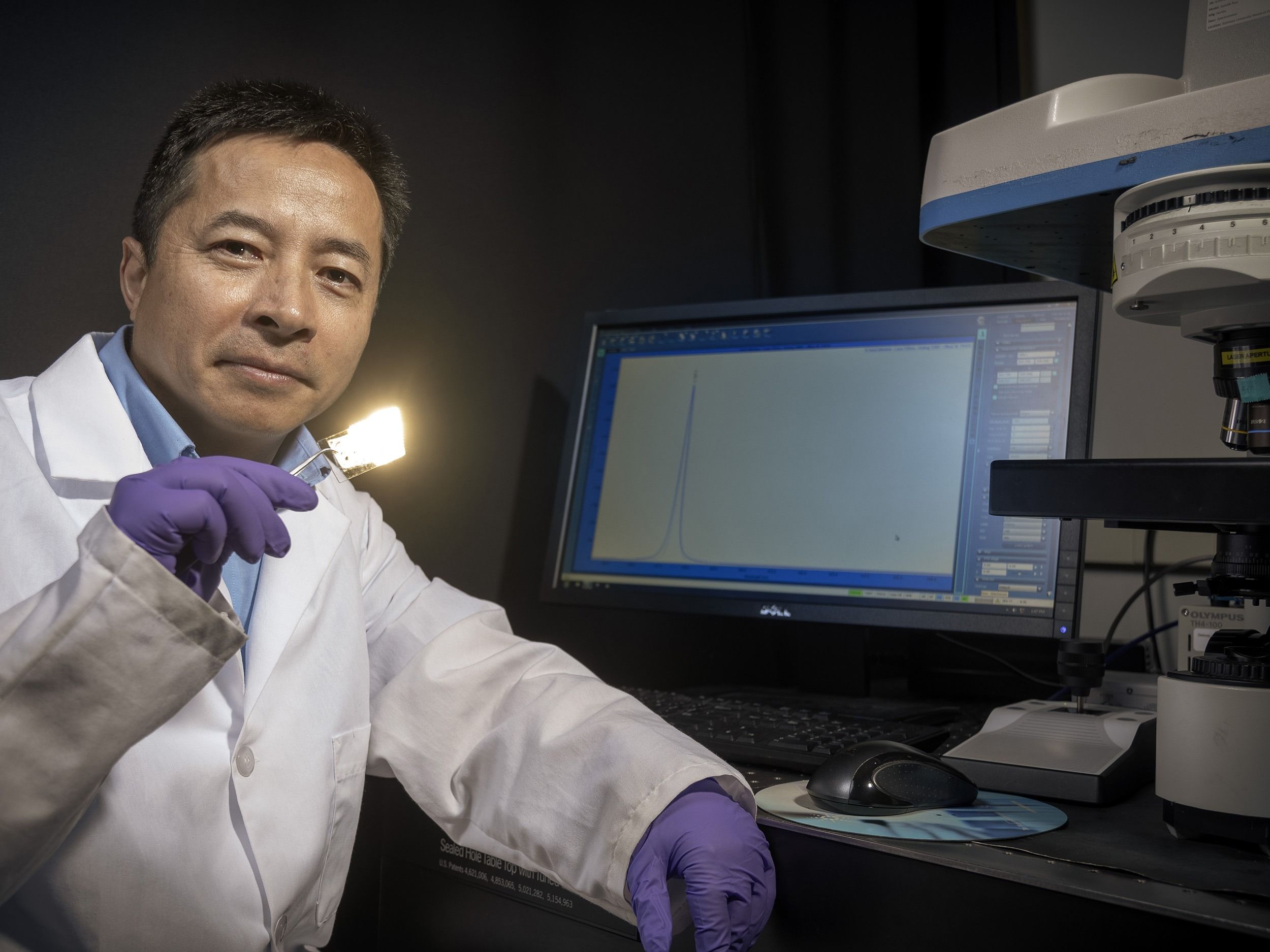
UNCG’s Dr. Jianjun Wei in the Joint School of Nanoscience and Nanoengineering has found a potential solution in a point-of-care biosensor built with nanostructures.
It all starts with biomarkers: substances in an organism whose presence, in this case, is indicative of disease.
Troponin, a family of proteins found in the cardiac and skeletal muscles, has been identified as a biomarker for CVD and can be measured in a simple blood sample. When the EKG results are inconclusive and patients head to the hospital for more blood work, this is the biomarker that medical professionals are looking at. But again, it takes too much time. And time is muscle.
Wei’s solution is a biosensor that, with the simple prick of a finger, would detect high troponin levels almost immediately, right at the scene.
The diagnostic device Wei (first photo below) and his collaborators are developing is a one-inch slide, etched with nanostructures a thousand times smaller than the width of a human hair.


As the use of manmade nanomaterials increases in modern life, scientists are beginning to wonder how these tiny structures will interact with our bodies and how they might impact our health. Recently, Wei began work with colleagues at North Carolina Central University on a $1 million NSF study of carbon nanodots. The tiny carbon particles appear to have antioxidant properties – like polyphenols in blackberries, they could help protect our cells from damage. One day, says Wei, carbon nanodots may be helpful in treating CVD and a host of other diseases. See more photos on UNCG Research Flickr.
Mabe (third photo above, left) says his experiences with Wilson and Guilford County Emergency Services played a major role in the evolution of the device plans. Wei and Mabe have completed over 200 customer discovery interviews.
In 2015, Wei received a $306,000 National Science Foundation (NSF) grant to focus on the first step in the process: perfecting the protein detection chip. In 2018, Wei’s team received a $50,000 NSF I-Corps grant to conduct customer discovery interviews and begin commercialization of their technology.
Wei and his team are designing the device specifically for the pre-hospital setting – for the paramedics and EMTs serving on the front lines. Wei is focused on the protein delivery and detection technology, while Dr. Taylor Mabe – who completed his Ph.D. in Wei’s lab in 2018 – serves as the entrepreneurial lead.
As Mabe gets feedback from potential customers and partners in the community, Wei makes appropriate changes to the chip, with additional guidance from Glenn Seymour, a senior-level sales and business development executive with decades of experience in bringing products like this to market.
In the fall, Mabe participated in a ride-along with Chris Wilson, Guilford County Emergency Services manager and public information officer. The experience showed Mabe just how chaotic these emergency situations can be – and how well the final device will need to hold up in these conditions.
“The device will need to be durable, easy to use, and accurate. It needs to withstand temperature changes and motion – these are things we didn’t think about at first,” Mabe says.
The goal is to complete the device in the next three to five years. Currently, the group is exploring a variety of funding opportunities to secure investment from a company with the engineering capabilities to design the device, which will include the sensor, a light source, a signal detector, and data processor.
Wei doesn’t view the biosensor as a replacement to current methods. Rather, it would be used as a complementary technology – one that would increase accuracy and save time.
Down the road, there could be broader applications.
“It’s not only for hospitals or medical professionals – it could be for individuals in their home,” Wei says. “Eventually, maybe it’s something that is integrated in your phone.”
Wei isn’t the only UNCG nanoscientist tackling cardiovascular health. Dr. Joseph Starobin has recently patented a new method of assessing how well our hearts are working. The associate professor, who is also an NSF I-Corps awardee, is working with Monebo Technologies, Rhythm Diagnostic Systems, and Unifi Manufacturing to develop the system into a wearable monitor of heart health.
From Lab to Life
Wei and Mabe began their commercialization journey locally, as members of the 2017 Greensboro I-Corps cohort.
UNCG and N.C. A&T’s joint Greensboro I-Corps program, part of the NSF’s Innovation Corps initiative and one of only four sites in the state, helps faculty, students, and alumni figure out the best real-world applications of their research. During the five-week program, researchers conduct interviews with potential customers, identify applications for their innovations, and then modify technology based on feedback. Successful teams might advance to the national I-Corps program, as Wei and Mabe did. They also have access to a strong startup framework at home.
This fall, UNCG received $100,000 from NC IDEA to launch a new program – NC I-Corps Next Step. The program will support scientists who have completed training at any of the four North Carolina I-Corps sites, in their company formation and fundraising efforts.
BACK TO THE BEGINNING
Let’s take a step back and rewind – from the 60-year-old with high CVD risk to the child who is just beginning to form healthy, or unhealthy, habits.
UNCG’s Dr. Laurie Wideman is adamant: When it comes to CVD, it matters what parents are doing with their children, and it starts younger than they may expect.
The Safrit-Ennis Distinguished Professor of Kinesiology is part of a team that is looking at how self-regulation – our ability to manage our emotions and behaviors appropriately – in childhood impacts cardiometabolic risk development in adolescents.
It’s a massive undertaking funded by a five-year, $3.6 million grant from the Eunice Kennedy Shriver National Institute of Child Health and Human Development. Yet it was a chance conversation between Wideman and fellow faculty member Susan Calkins that sparked the work.
Calkins and a team had been working for years on the RIGHT Track study, a project examining self-regulation and psychosocial outcomes in children over time. The human development and family studies professor had noticed that many of the children were becoming obese, and she began to wonder if there was a relationship between obesity and self-regulatory behaviors.
“Susan mentioned some of the results, and said she wasn’t exactly sure what was going on,” Wideman said. “I thought, ‘this is amazing – no one in our field has this kind of rich data set involving hundreds of families across time.’”
Wideman teamed up with Calkins and other UNCG researchers – Dr. Cheryl Lovelady and Dr. Lenka Shriver in nutrition, Dr. Susan Keane in psychology, and former UNCG Professor Lilly Shanahan – to focus on health outcomes in a second study: RIGHT Track Health.
There is a lot of data in human development literature regarding self-regulation, but very little on related health outcomes.
In kinesiology, there’s been significant work on health-related cardiometabolic risk in adolescence. “But what our field is lacking is historic information about why certain kids may have higher risks than others,” Wideman says.
“This study allows us to look at this problem from a cross-disciplinary perspective.”
Here’s what they’ve found so far: Children who have poor self-regulation are more likely to have poor cardiometabolic outcomes – obesity, hypertension, insulin resistance, etc. – in adolescence. Children that showed high emotion regulation at age two only had a 5.5 percent chance of being in the high risk cardiometabolic group 14 years later.
“It makes sense that children who have trouble regulating emotion and behavior may not be good at regulating what they eat, how much sleep they get, and how active they are,” says Wideman.
Wideman’s team is now working to secure additional funding to follow these individuals into adulthood. Ultimately, the goal is to develop prevention and intervention strategies that help people become better self-regulators and minimize poor health outcomes.
But that’s still years down the road. Given the study’s findings, what should parents be doing now?
“We have to help our kids be better self-regulators,” Wideman says. “It will look different for every child, but parents should be aware of this. It’s important that we start to pattern healthy habits for our kids.”
With more than $10 million in National Institutes of Health funding, the UNCG RIGHT Track study has examined emotion regulation and development in children from 450 families, across two decades.



As RIGHT Track participants enter young adulthood, Wideman (second photo, center) and her students track their fitness – measuring oxygen consumption, using “the Bodpod” to assess body fat (third photo), and more. In her work, Wideman uses the term “cardiometabolic risk” instead of cardiovascular risk. Factors like obesity and high blood pressure, she explains, up your chances for diabetes as well as heart disease and stroke. See more photos on UNCG Research Flickr.
INCREASED RISK
There’s no one-size-fits-all approach for CVD interventions – different groups of people have varying needs.
Dr. Qibin Zhang is another UNCG researcher working with biomarkers in blood, but he’s looking beyond troponin to identify other proteins that can best predict CVD for individuals with type 1 diabetes.
If you have type 1 diabetes, your risk for CVD increases by two- to four-fold, and only half of this excess risk is explained by known factors. That’s why Zhang and his team at UNCG’s Center for Translational Biomedical Research at the NC Research Campus are working to detect novel biomarkers that can explain why these individuals have such a higher risk.
“If we can detect the biomarkers before the symptoms appear, then interventions could be applied early on to prevent a heart attack,”
Zhang says.
Zhang’s research lab is focused on glycated proteins, or proteins modified by sugars, as potential markers for CVD and other diabetic complications. With a pilot grant from the Helmsley Charitable Trust in 2015, Zhang’s team developed a technique to accurately measure glycated proteins in human plasma. The pilot’s success has resulted in two large, three-year grants to further the research: $496,000 from the American Heart Association and $742,000 from the National Institutes of Health.
It’s work that has the potential to impact millions of lives – type 1 diabetes affects approximately 1.4 million people in the United States and 30 million people globally. CVD is the main cause of death for individuals with type 1 diabetes, and often CVD occurs earlier in life for this population.
“The ultimate goal is to be able to cure these horrible diseases,” Zhang says. “This is work that spans generations – it takes generations of scientists to address these issues.”
TAKING ACTION
It’s been called the “silent killer of women.”
“Women’s No. 1 health threat.”
Often, it’s our fathers, brothers, husbands, and sons who worry about CVD. But it’s also the number one killer of women worldwide.
When it comes to recognizing symptoms, identifying a heart attack, and getting the appropriate care, the stats are unsettling: On average, women delay 30 minutes longer than men in seeking treatment. And every 30-minute delay increases mortality risk by 7.5 percent.
The longstanding myth is that women ignore symptoms because they are in denial or too busy caring for others. But Dr. Leslie Davis, a longtime nurse turned UNCG associate professor who has dedicated years to this research, says no.
“It all starts with recognizing symptoms, interpreting them, and then acting,” she says. “My research and that of others have shown that this process is complicated.”
In general, women are less likely to experience chest pain than men, and have a greater number of symptoms. And for women who have had a heart attack, symptoms of a second or third attack may differ from the first.
“Women aren’t just sitting at home – they’re doing a lot of work mentally to recognize and interpret what’s going on.”
Davis’ approach is unique in that it focuses on teaching women the skills to identify and interpret symptoms. Over the past several years, she’s been piloting an educational intervention study – funded by a Sigma Theta Tau International Honor Society of Nursing grant and two UNCG faculty grants – in which she goes into the homes of women who are heart attack survivors and teaches them how to recognize and interpret symptoms.
Why focus on women who have already experienced a heart attack? Because one in five of these women will have another heart attack within a year, Davis says.
If women can accurately recognize and interpret symptoms, they are more likely to take appropriate action – which often means calling 911.
“If you have had a heart attack, and you feel symptoms that you believe are heart-related, you need to call 911,” Davis says. “Most people think their spouse can drive them to the hospital quicker. But it’s important to call an ambulance because you can get life-saving treatment in the ambulance. Once you arrive at the hospital, the medical team will be prepared.”
Davis is translating her findings for health care providers, so they too understand the issues surrounding recognition of symptoms.
“Many women have symptoms that are slow and intermittent, and health care providers need to realize that these symptoms can still be indicative of a heart attack. I’ve found that even knowledgeable nurse practitioners have recommended that patients drive to the hospital instead of calling 911, because the symptoms didn’t seem that bad.”
The next step? A randomized control experiment to test the effectiveness of the educational intervention with a larger group.
“It’s a great time to make a difference in health care, particularly with women,” she says. “If this educational intervention works, it could change what we do across the nation.”
